In this article, I’m going to explore an independent marker for heart disease that you may not have heard of and is rarely tested in the UK. This marker is Lipoprotein(a). I will discuss what it is, what different levels are and how to manage it if you have raised levels.
Cardiovascular disease (CVD) is the leading cause of death and a reduced healthspan. Managing and reducing the risk of CVD is, therefore, essential to a long and healthy life.
The healthy guy who drops dead from a heart attack

We’ve all heard of that healthy person, who suffers a fatal heart attack out of the blue. It turns out they had significant CVD despite an optimal lifestyle. Why?
Well, Lp(a) is one of those silent killers we can be completely unaware of. In most cases, we can assume that if you lead a healthy lifestyle with a good diet, regular exercise, don’t smoke and limit alcohol intake you have a significantly lower risk of CVD.
However, this is not the case if you are genetically predisposed to having a raised Lp(a) because this marker is driven more by genetics than lifestyle. If you have a raised Lp(a) then it is even more important to make sure your LDL-C and ApoB remain at healthy levels. If it is very high, then you may want to seek out specialist treatment.
And, if you are in your late 40’s or if you have had a close relative have premature CVD, you may want to consider doing further investigations like a coronary artery calcium scan to check your status.
What is Lipoprotein(a)?
Lipoprotein(a), or Lp(a), was discovered in the early 1960s by Norwegian physician and researcher Kaare Norum. The discovery of Lp(a) added a significant piece to the puzzle of lipid metabolism and its relation to cardiovascular disease.
We know that some people with healthy LDL-C (aka the bad cholesterol) still get CVD, but why? Lp(a) is a significant player that can exist at high levels, increasing the risk even when your LDL levels ar normal.
Each LDL (Low-Density Lipoprotein) particle contains one Apolipoprotein B (ApoB) molecule. However, a unique type of lipoprotein called Lipoprotein(a), or Lp(a), can be attached to some LDL particles. This addition of Lp(a) is concerning because it makes these LDL particles more harmful to our blood vessels, increasing the risk of cardiovascular diseases.
It is a key factor even in individuals who lead a healthy lifestyle as it can be resistant to diet and lifestyle modifications. It can also be difficult to treat medically.
It is an independent risk factor for cardiovascular disease meaning that if it is high and your other cholesterol markers like LDL are low, you still have an increased risk of CVD.
In the UK, no therapeutic management is currently agreed upon (see treatment options below).
What is it about lipoprotein(a) that makes it a problem?
- Sticky Nature: Lp(a) is stickier than other types of cholesterol particles, making it more likely to cling to the walls of blood vessels. This can lead to the formation of plaque, a thick, hard deposit that can narrow or block arteries.
- Promotes Clotting: Lp(a) can interfere with the body's ability to dissolve blood clots. This means that not only can it contribute to building up plaques, but it can also make existing plaques more likely to lead to dangerous clots.
- Mimics Helpful Proteins: Part of Lp(a) resembles a protein that helps repair tissues, including blood vessel walls. Because of this, it can accumulate in the arteries under the guise of helping, but instead, it contributes to plaque buildup.
.
Should I test for Lp(a)?
 The European Society of Cardiology recommends that adults should be checked at least once in their lifetime. A consensus statement in the UK also recommends testing for anybody who has:
The European Society of Cardiology recommends that adults should be checked at least once in their lifetime. A consensus statement in the UK also recommends testing for anybody who has:
What is a high lipoprotein(a) level?*
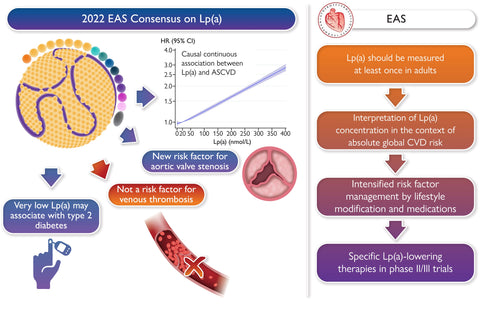
in 2022 the European Atherosclerosis Society produced a consensus statement on what constitutes an increased risk.
As you can see from the diagram, it is a linear association. Other risk factors should also be considered when considering treatment. For example, a person with a high LDL-C and high lipo(a) is at high risk. However, if the LDL-C is reduced, the combined risk moves them into a lower-risk category.
A high Lipoprotein(a), or Lp(a), level is considered a risk factor for cardiovascular diseases*. In terms of nmol/L, an Lp(a) level is generally interpreted as follows:
- Low risk: Less than 25 nmol/L
- Mild risk: 25-75 nmol/L
- Moderate risk: Greater than 75-125 nmol/L
- High risk: Greater than 125 nmol/L
*Updated April 2024 to European Consensus guidelines
When assessing overall risk it is important to take into account other factors ie raised LDL-C, family history of heart disease, BMI, blood pressure etc.
It's important to note that the specific cut-off values can vary slightly by laboratory and the guidelines used. However, most experts agree that levels above 50 nmol/L increase cardiovascular risk, and levels above 125 nmol/L are associated with a significantly higher risk of atherosclerotic cardiovascular diseases, such as heart attack and stroke.
*Note: The concentration of Lp(a) is typically measured in milligrams per deciliter (mg/dL) or nanomoles per liter (nmol/L), depending on the region and the lab's practices. Due to differences in the molecular weight of Lp(a) particles among individuals, nmol/L is often considered a more standardised measure.
When should I consider having it treated?
Anyone with a level over 50 should make sure that they optimise their diet and lifestyle (see section below).
In the UK the threshold for treatment is when levels are >90 nmol/L, in the US this cut off is higher at >125 nmol/L.
However, if your levels are between 50-125 you may want to consider further analysis to look at the health of your arteries.
What other tests might I consider to check my cardiovascular health?
If you have a raised level, you may want to consider checking the health of your blood vessels before considering any treatment. Checking the health of the blood vessels around the heart to look for heart disease and the carotid artery that supplies the brain will determine if there is a risk for stroke or heart issues.
- Carotid Ultrasound: This test uses sound waves to create images of the carotid arteries in your neck and can detect plaque buildup or blockages that could lead to a stroke.
- CAC test: Coronary artery calcium score/ scan: This test is a CT scan to detect calcification in the coronary arteries and is becoming increasingly popular. A high score indicates a higher risk of coronary artery disease. These tests cost around £4-600 in the UK and are easily available through several private health care providers.
- Ankle-Brachial Index (ABI): This test compares the blood pressure readings in your ankle and your arm to identify peripheral artery disease (PAD). In this condition, the arteries in the legs are narrowed or blocked.
- Magnetic Resonance Imaging (MRI) and Cardiac CT: These imaging tests provide detailed images of the heart and blood vessels, helping to identify problems such as heart disease, congenital heart defects, and plaque buildup in the arteries. They can be done at a specialist heart centre.
- Blood Tests: Beyond Lp(a), additional blood tests can provide information about other risk factors for heart disease, such as cholesterol levels, triglycerides, high-sensitivity C-reactive protein (hs-CRP), Apo B and LDL particle size.
Genetics of Lp(a)
The levels of Lp(a) in the blood are highly heritable and are primarily determined by the LPA gene on chromosome 6, which encodes the apolipoprotein(a) component of Lp(a).
It is variations in the LPA gene that determine the plasma concentration and size of the Lp(a) particles. The most significant genetic variations influencing Lp(a) levels are related to the number of kringle IV type 2 (KIV-2) repeats in the apolipoprotein(a) gene. Individuals with a lower number of KIV-2 repeats tend to have higher Lp(a) levels, while those with a higher number of repeats tend to have lower Lp(a) levels.
SNPs and Lp(a) Levels
Several single nucleotide polymorphisms (SNPs) in the LPA gene have been associated with Lp(a) levels and cardiovascular risk. Some SNPs affect the kringle IV type 2 repeat number, while others influence Lp(a) levels through different mechanisms.
- rs10455872: This SNP is located in the LPA gene and has been associated with increased Lp(a) levels and a higher risk of coronary artery disease.
- rs3798220: Another SNP in the LPA gene, rs3798220, has been linked to increased Lp(a) levels and cardiovascular disease risk.
Treatment for lowering Lp(a)
Unlike other lipoprotein levels, Lp(a) levels are largely determined by genetics and less influenced by lifestyle changes. However, certain dietary and lifestyle modifications can help manage overall cardiovascular risk and may have a modest impact on lowering Lp(a) levels or mitigating its effects.
Dietary Modifications
- Reduce Saturated and Trans Fats: Limit foods high in saturated and trans fats, such as red meat, butter, cheese, and processed foods, to help lower LDL cholesterol levels, which can indirectly influence cardiovascular risk associated with high Lp(a) levels.
- Increase Intake of Omega-3 Fatty Acids: Foods rich in omega-3 fatty acids, like salmon, mackerel, walnuts, and flaxseeds, can have a positive effect on heart health by reducing triglycerides and potentially influencing Lp(a) levels.
- Eat More Fibre: High-fibre foods, such as fruits, vegetables, whole grains, and legumes, can help reduce cholesterol absorption in the intestine and improve overall cholesterol levels.
- Niacin (Vitamin B3): While niacin can lower LDL cholesterol and triglycerides, its effect on Lp(a) levels is inconsistent. High doses can reduce Lp(a) levels, you should check with your Doctor before considering high-dose niacin (see treatment below and references for more info.)
- Antioxidant-rich Foods: Consuming foods high in antioxidants, like berries, nuts, green leafy vegetables, and whole grains, may help combat oxidative stress and inflammation associated with high Lp(a) levels.
Lifestyle Modifications
- Regular Exercise: Engaging in regular aerobic exercise, such as walking, cycling, or swimming, can improve overall cardiovascular health, though its direct effect on lowering Lp(a) levels is limited.
- Maintain a Healthy Weight: Achieving and maintaining a healthy weight can help reduce the risk of cardiovascular disease and improve lipid profiles, indirectly affecting the risk associated with Lp(a).
- Avoid Smoking: Smoking cessation is crucial as smoking exacerbates cardiovascular risk, especially in individuals with high Lp(a) levels.
- Limit Alcohol Consumption: Moderate alcohol consumption is advised since excessive intake can negatively affect lipid levels and cardiovascular health.
- Manage Stress: Chronic stress can adversely affect cardiovascular health, so adopting stress-reduction techniques (e.g., mindfulness, yoga, regular exercise) can be beneficial.
Medical Intervention
In cases where Lp(a) levels are significantly high, and there is a substantial risk of cardiovascular disease, medication then medical interventions may be required.
Medical Interventions to Manage High Lp(a) and Cardiovascular Risk
- Niacin (Vitamin B3): High doses of niacin have been shown to lower Lp(a) levels in some people, but its impact on reducing cardiovascular events is uncertain. It should only be used under medical supervision due to potential side effects.
- PCSK9 Inhibitors: Although primarily used to lower LDL cholesterol, some studies suggest that PCSK9 inhibitors can also reduce Lp(a) levels. These are prescription medications given as injections and ar available through the NHS.
- Lipoprotein Apheresis: A process similar to dialysis, where blood is filtered to remove Lp(a) particles, recommended for very high levels of Lp(a) and existing cardiovascular disease. It's effective but costly and requires regular sessions. Currently, it is used for people who have all 3 of: a. familiar hypercholestrolaemia (FH) b. Very raised LDL-cholesterol and c. Coronary artery of peripheral artery disease.
Read more about Lipoprotein apheresis at the Royal Brompton Hospital.
- Aspirin: While not directly lowering Lp(a) levels, aspirin may be recommended to reduce the risk of clotting in individuals with high cardiovascular risk.
Future Prospects for treatment
Antisense oligonucleotides and siRNA therapies hold promise for managing conditions like high Lp(a) levels, where traditional treatments have been limited or ineffective.
Antisense Oligonucleotides (ASOs)
- Mechanism: ASOs are short, synthetic strands of nucleotides designed to specifically bind to the mRNA transcripts encoding for the Lp(a) protein. By binding to these mRNA transcripts, ASOs prevent the translation process, reducing the production of Lp(a) protein.
- Development and Use: ASOs targeting Lp(a) are in various stages of clinical development. They have shown promise in significantly lowering Lp(a) levels in the bloodstream by targeting the genetic production process directly. One example is APO(a)-LRx, which has demonstrated effectiveness in lowering Lp(a) levels in preliminary studies.
Small Interfering RNA (siRNA) Therapies
- Mechanism: siRNA therapies work by utilizing small interfering RNA molecules to silence specific genes involved in the production of proteins like Lp(a). These siRNA molecules are designed to be complementary to the mRNA of the target protein, leading to the degradation of the mRNA and thus preventing the protein's production.
- Development and Use: siRNA therapies for reducing Lp(a) levels are also under investigation, with some showing promising results in early clinical trials. Inclisiran is an siRNA therapy targets PCSK9 to lower LDL cholesterol, and its success has paved the way for exploring siRNA-based treatments for Lp(a).
Advantages and Considerations
- Targeted Therapy: Both ASOs and siRNA therapies offer targeted approaches to lower Lp(a) levels, potentially reducing cardiovascular risk without significantly affecting other lipid levels or causing broad systemic side effects.
- Long-Lasting Effects: These therapies may provide long-lasting effects with less frequent dosing compared to traditional medications.
- Clinical Trials and Approval: Several of these therapies are still in clinical trials, and their long-term efficacy and safety are being studied.
Is there a link between lipoprotein (a) and dementia/ cognitive decline?
A study published in Nature Scientific Reports examined the relationship between lipoprotein (a) and cognitive function. Based on data from the Berlin Agin Study II, there is some weak evidence that men with a raised Lp(a) have a decreased cognitive function regardless of their APOE status.
References
- Tsimikas S. A Test in Context: Lipoprotein(a): Diagnosis, Prognosis, Controversies, and Emerging Therapies. J Am Coll Cardiol. 2017;69(6):692-711. doi:10.1016/j.jacc.2016.11.042
- Reyes-Soffer G, Ginsberg HN, Berglund L, et al. Lipoprotein(a): A Genetically Determined, Causal, and Prevalent Risk Factor for Atherosclerotic Cardiovascular Disease: A Scientific Statement From the American Heart Association. Arterioscler Thromb Vasc Biol. 2022;42(1):e48-e60. doi:10.1161/ATV.0000000000000147
- Familyheart.org How to treat high Lp(a)
- Current management of the patient with high lipoprotein(a)
- The British Journal of Cardiology March 2022
- Kronenberg F, Mora S, Stroes ESG, et al. Lipoprotein(a) in atherosclerotic cardiovascular disease and aortic stenosis: a European Atherosclerosis Society consensus statement.
- Parhofer KG, Laufs U. Lipid Profile and Lipoprotein(a) Testing. Dtsch Arztebl Int. 2023;120(35-36):582-588. doi:10.3238/arztebl.m2023.0150 Eur Heart J. 2022;43(39):3925-3946. doi:10.1093/eurheartj/ehac361
- Greenland P, Blaha MJ, Budoff MJ, Erbel R, Watson KE. Coronary Calcium Score and Cardiovascular Risk. J Am Coll Cardiol. 2018;72(4):434-447. doi:10.1016/j.jacc.2018.05.027
- Stivalet O, Paisant A, Belabbas D, et al. Combination of Exercise Testing Criteria to Diagnose Lower Extremity Peripheral Artery Disease. Front Cardiovasc Med. 2021;8:759666. Published 2021 Nov 17. doi:10.3389/fcvm.2021.759666
- Schmidt K, Noureen A, Kronenberg F, Utermann G. Structure, function, and genetics of lipoprotein (a). J Lipid Res. 2016;57(8):1339-1359. doi:10.1194/jlr.R067314
- Svilaas T, Klemsdal TO, Bogsrud MP, et al. High levels of lipoprotein(a) - assessment and treatment. Høyt nivå av lipoprotein(a) – utredning og behandling. Tidsskr Nor Laegeforen. 2022;142(1):10.4045/tidsskr.21.0800. Published 2022 Dec 16. doi:10.4045/tidsskr.21.0800
- Sahebkar A, Reiner Ž, Simental-Mendía LE, Ferretti G, Cicero AF. Effect of extended-release niacin on plasma lipoprotein(a) levels: A systematic review and meta-analysis of randomized placebo-controlled trials. Metabolism. 2016;65(11):1664-1678. doi:10.1016/j.metabol.2016.08.007
- O'Donoghue ML, Fazio S, Giugliano RP, et al. Lipoprotein(a), PCSK9 Inhibition, and Cardiovascular Risk. Circulation. 2019;139(12):1483-1492. doi:10.1161/CIRCULATIONAHA.118.037184
- Chan DC, Watts GF. The Promise of PCSK9 and Lipoprotein(a) as Targets for Gene Silencing Therapies. Clin Ther. 2023;45(11):1034-1046. doi:10.1016/j.clinthera.2023.07.008
- Langsted A, Nordestgaard BG. Antisense Oligonucleotides Targeting Lipoprotein(a). Curr Atheroscler Rep. 2019;21(8):30. Published 2019 May 20. doi:10.1007/s11883-019-0792-8
- Lipoprotein apheresis at the Royal Brompton Hospital.
- Röhr F, Bucholtz N, Toepfer S, et al. Relationship between Lipoprotein (a) and cognitive function - Results from the Berlin Aging StudyII. Sci Rep. 2020;10(1):10636. Published 2020 Jun 30. doi:10.1038/s41598-020-66783-3
- Florian Kronenberg, Samia Mora, Erik S G Stroes, Brian A Ference, Benoit J Arsenault, Lars Berglund, Marc R Dweck, Marlys Koschinsky, Gilles Lambert, François Mach, Catherine J McNeal, Patrick M Moriarty, Pradeep Natarajan, Børge G Nordestgaard, Klaus G Parhofer, Salim S Virani, Arnold von Eckardstein, Gerald F Watts, Jane K Stock, Kausik K Ray, Lale S Tokgözoğlu, Alberico L Catapano, Lipoprotein(a) in atherosclerotic cardiovascular disease and aortic stenosis: a European Atherosclerosis Society consensus statement, European Heart Journal, Volume 43, Issue 39, 14 October 2022, Pages 3925–3946