The intelligent way to utilise GLP-1 is through microdosing and augmenting its effectiveness.
GLP-1 medications are making a profound difference in my practice; however, they are being used incorrectly as a whole.
As a UK-based functional and longevity doctor, I've seen firsthand their profound impact on patients, not just in shedding pounds, but in changing how they behave around food and even improving mental well-being.
These are powerful tools, particularly in their ability to quiet "food noise" and, as evidence suggests, even support conditions like ADD and alcohol dependency.
However, a critical danger lurks beneath the surface of this excitement: these medications are being misused.
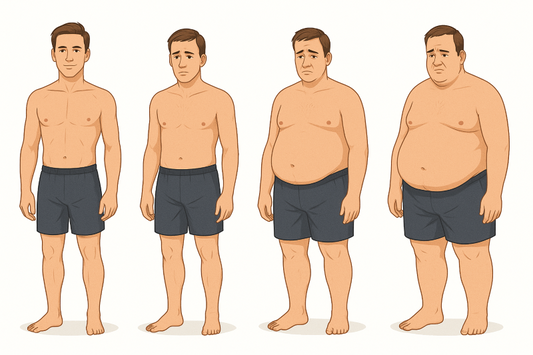
Many approaches focus solely on the immediate outcome- weight loss - without addressing the fundamental underlying physiological imbalances. This narrow view is why some patients fail to achieve sustainable results, why others experience significant rebound weight gain, and why some eventually become resistant to the medication's effects.
The incomplete picture: calories in, calories out is wrong
While the theory that weight loss is simply "calories in, calories out" exists, it is only part of the picture. This view often overlooks the crucial role of hormones in how our bodies process, store, and utilise energy.
My clinical experience, supported by detailed blood tests, hormone panels, and DEXA scans, consistently points to a more nuanced reality: calories plus hormones. This is the crucial element that is often overlooked when it comes to GLP medication, and it's precisely why a significant number of patients struggle to maintain their progress.
Insulin resistance and "fat resistance" are the key to long-lasting results
Let's delve into the hormonal aspect. When we consistently experience glucose spikes, our bodies respond by producing more insulin. Over time, this chronic overproduction leads to a state known as insulin resistance, where the body becomes accustomed to high insulin levels, resulting in resistance.
Now, what does insulin do? Insulin causes fat resistance. It locks the fat inside the cells. This means that even if you're carrying excess weight, your body struggles to access that stored fat for energy. It's as if your fat cells are locked away, inaccessible, despite your body's energy needs.
Imagine this scenario: you're in a state of locked-up fat, and then you embark on a calorie-restricted diet. Your body is now in a calorie deficit, hunting for energy.
Can it get it from your locked-up fat cells? A little, perhaps, but not very much, because the strong message from insulin is still "store fat."
So, where does your body turn for energy? It starts breaking down muscle.
The peril of muscle loss: A hidden cost of uninformed weight loss
This is the key to why patients often lose a significant amount of muscle. It's very easy to be in a calorie deficit because you no longer get the hunger pangs.
Losing muscle compromises your strength, mobility, and overall long-term health.
Many patients on GLP-1s report feeling less hungry, making it easier to adhere to a calorie deficit.
They step on the scales, see the numbers drop, and celebrate. However, what they often lose is not just fat, but also muscle. They hit their "target weight," come off the GLP-1, and then the inevitable happens.
Because the underlying insulin resistance hasn't been addressed, their hunger returns immediately. They start overeating. They put all the weight back on again. This is the dreaded rebound effect, and it's a direct consequence of a superficial approach to weight loss.
The solution: A hormonal reset for sustainable success
The answer lies in a more intelligent, holistic approach. We can, and should, measure insulin resistance. This isn't just about advanced diagnostics; even basic blood markers can offer crucial insights. Once we understand the degree of insulin and fat resistance, we unlock a "golden window" of opportunity.
This window enables us to utilise GLP-1 medications to enhance insulin sensitivity. When your body becomes more sensitive to insulin, it can more easily release stored fat for energy, even without enormous calorie deficits. This means:
-
Lower doses, better effects: You can use significantly lower doses, achieving more effective results.
-
Reduced muscle loss: You experience lower muscle loss.
-
Enhanced sustainability: By addressing the root cause, insulin resistance, you establish a foundation for long-term weight management, significantly reducing the risk of rebound when you eventually taper off the medication.
Furthermore, by taking an intelligent approach to supplementation, it is possible to reduce muscle loss and further enhance results, ultimately leading to a more favourable outcome.
The way many GLP-1 studies were conducted focused on "quickest weight loss." But that is not the way to do it.
Beyond the number on the scale: the bigger picture
In summary, for truly impactful, long-term health, we must:
-
Understand and reverse fat resistance: This involves addressing insulin resistance.
-
Utilise GLP-1s strategically: Employ them as a tool to improve insulin sensitivity and manage appetite, rather than just a blunt instrument for calorie restriction, and stay on low doses.
-
Prioritise muscle preservation: Actively work to maintain and build muscle mass throughout the weight loss journey.
-
Stay on lower, effective doses: Optimise the medication's benefits while minimising risks.
The implications of this approach extend far beyond aesthetics. Obesity causes lots of issues; it drives increased inflammation, autoimmune disease, and cancer. By addressing the underlying hormonal imbalances and achieving sustainable, healthy weight loss, we're not just improving how you feel today; we're profoundly impacting your long-term health trajectory and longevity.
What if we reframed weight loss not as a battle against calories, but as a journey to restore hormonal harmony?
By utilising this way, we can reduce dangerous visceral fat, which drives down inflammation.
Insulin resistance is also key to high LDL cholesterol levels, so by treating at the root cause of the problem we can improve this as well, all whilst using lower doses or microdosing with this game-changing medication.
Dr Geoff Mullan
This scientific article is for educational purposes only and does not constitute medical advice. Using any medication should be done under the guidance of a medical professional.