For too long, our approach to weight management has been dictated by numbers – specifically, the Body Mass Index (BMI). In today’s age of rapidly expanding use of GLP medications, our focus seems to have shifted towards a one-size-fits-all model. This model not only misinterprets who should be receiving these interventions but also overlooks critical factors such as metabolic health, insulin resistance, and overall nutrition. As a functional and longevity doctor, I have witnessed firsthand the pitfalls of relying solely on BMI to gauge health. It is time we revisit these assumptions and develop a more effective, personalised approach that addresses the true drivers of metabolic dysfunction.
The BMI myth
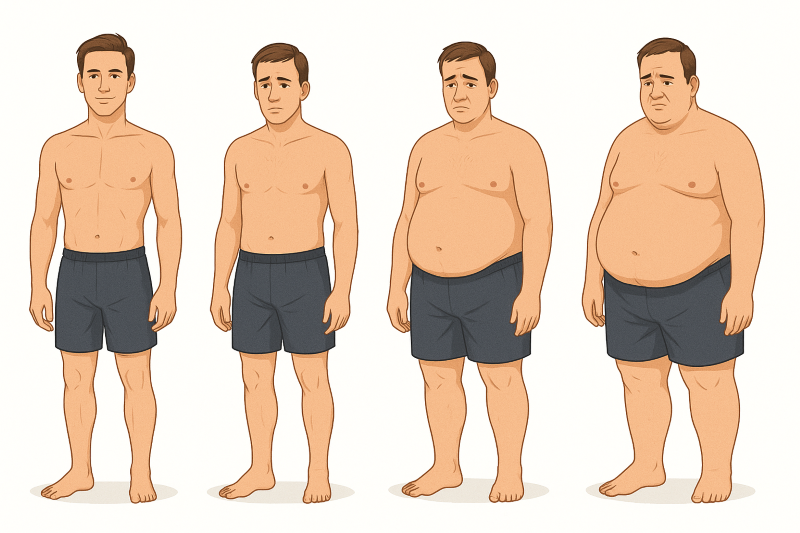
BMI has become the de facto standard in many clinical settings for identifying when weight becomes “unhealthy”. Conventionally, a BMI over 30 is flagged as the cutoff for obesity, and over 27 with comorbidities like hypercholesterolemia. But as we increasingly see, this isn’t an accurate gauge for everyone. Consider the case of someone like Mario Itoje the England rugby captain – despite having a BMI in the obese range (around 32), his body fat percentage is only 9%, and his metabolic profile remains exceptional as an elite athlete. This disconnect highlights a major issue: BMI is a crude tool and does not account for metabolic health. There are many people for whom BMI is misleading. If we were to shift our focus to what truly causes weight gain, insulin dynamics become the clear culprit.
Insulin: The metabolic gatekeeper
Weight gain fundamentally begins when insulin pushes glucose into fat cells, effectively turning it into stored fat. A diet rich in carbohydrates prompts frequent spikes in insulin, which over time may lead to insulin resistance. High fasting insulin and elevated HOMA-IR scores can be detected four, five, or even six years before an individual reaches a supposedly “unhealthy” BMI. In essence, metabolic dysfunction is set in motion long before we see the numbers on a scale or BMI chart. This early warning system is crucial; it allows for intervention at a stage where lifestyle changes and measured nutritional support can have a profound impact.
Traditionally, drug trials for weight loss medications have aimed at rapid weight loss, focusing on how much weight can be lost the fastest. Yet, this strategy is problematic as it often results in drastic caloric deficits that can lead to muscle loss and malnourishment. Instead of simply asking: “Can this drug help you lose weight quickly?” we should be investigating how to guide patients into a state of nutritional balance, where they do not experience constant cravings, unhealthy snacking, or alcohol consumption. In doing so, we embrace a proactive approach to health rather than a reactive one, supporting patients with nutrition and, if needed, short-term, lower-dose medications to avoid large hypocaloric gaps.
A new paradigm for weight management
The promise of GLP-based medications has been widely celebrated in recent months. But if these drugs are primarily used in individuals with a high BMI – rather than those with metabolic dysfunction – we risk missing the real beneficiaries. Our treatment protocols must evolve to target the real issue at its metabolic roots. This means:
· Measuring fasting insulin and HOMA-IR scores to detect metabolic dysfunction early, sometimes years before BMI becomes elevated.
· Carefully adjusting nutritional intake based on individual macro- and micronutrient needs, supporting patients to eat in a healthier way and avoid overeating.
· Providing short-term, lower-dose medications where necessary to support lifestyle changes, rather than relying on long-term, high-dose regimens that may benefit pharmaceutical companies more than patients.
· Using advanced AI tools to tailor dietary recommendations for optimal metabolic health, including calculating precise macronutrient and nutrient needs.
By focusing on metabolic health rather than just weight, we can reduce the incidence of the two leading causes of death – cardiovascular disease and dementia. Metabolic health is central to both: cardiovascular disease is the number one cause of death, and dementia is closely linked to metabolic dysfunction and apolipoprotein E4. Notably, statins, often prescribed for cardiovascular risk, can themselves contribute to insulin resistance, raising questions about their role in metabolic health. Addressing these factors holistically is not only more effective but also more sustainable in the long term.
The role of technology and personalisation
Modern technology offers us an unprecedented opportunity to personalise treatment protocols. With AI-driven analytics, it is now possible to calculate exactly what each patient needs in terms of caloric intake, nutrient balance, and even the timing of meals. These innovations give us the ability to monitor metabolic parameters continuously, adjusting treatments as required. This is a significant departure from the traditional “trial and error” approach that has dominated weight management trends for decades.
This technology-enhanced approach places the patient – and not the pharmaceutical company – at the centre of treatment. Rather than designing protocols that primarily benefit the industry, we are now crafting strategies that benefit the individual. It is essential that our protocols reflect this paradigm by shifting from a ‘one size fits all’ mentality to an individualised blueprint for health.
Looking to the future
What does the future hold for weight management and metabolic health? It is clear that our approach must change. The current use of GLP medications exemplifies this shift – moving from a weight-centric framework to a health-centric one. We must invest in educating both practitioners and the general public about the underlying metabolic derangements that precede an unhealthy BMI. If we can identify and correct insulin resistance early, we can stave off the cascade of metabolic disruption that eventually leads to chronic disease.
As practitioners, we are in a unique position to champion this change. We have the tools, the research, and the clinical experience to direct our patients towards better health outcomes. In the race against time in functional and longevity medicine, every early intervention counts. The challenge now is not solely to lose weight but to ensure that the weight lost is a step towards reclaiming true metabolic health, with a focus on preserving muscle mass and preventing malnutrition.
Call to Action
I urge my fellow clinicians and wellness enthusiasts to rethink our current standards. It’s time we measure metabolic health and use that data to inform our treatment of weight management. Let’s not reduce the human body to a number but understand the complex interplay of hormones, diet, and lifestyle that defines our well-being.
Dr Geoff Mullan
This opinions are my own and do not constitute medical advice.